02/01/2026
As we enter February, it is an ideal time to build upon the New Year focus on health by examining one of the most foundational systems in the body: the immune system. Immune resilience is not determined by a single supplement or intervention, but rather by the cumulative effects of nutrition, lifestyle behaviors, and gut health across the lifespan.
This topic was the focus of my recent JOY106.3FM Healthy Segment, where we discussed how immune health is deeply interconnected with the gut microbiome and daily lifestyle choices from birth through older adulthood.
Listen to the full radio segment here: https://youtu.be/SUA4JFmrE5M?si=CMR1kGH3aU1OSXqi&t=540
The Gut–Immune Connection
Approximately 70% of the immune system resides within the gut, making the gastrointestinal tract a central hub for immune regulation. The gut is home to the microbiome, a complex and dynamic ecosystem of microorganisms—including bacteria, viruses, fungi, and yeast—that play essential roles in:
- Protecting against infections
- Supporting nutrient absorption
- Regulating inflammation
- Influencing metabolic, neurologic, and mental health
The microbiome begins forming at birth and continues to evolve throughout life. While early exposures matter, the microbiome is highly adaptable, responding continuously to dietary patterns, stress levels, sleep quality, physical activity, medication use, and environmental exposures.
Nutrition as a Primary Immune Modulator
From a Lifestyle Medicine perspective, dietary quality is one of the most powerful tools for supporting immune health.
Emphasize Prebiotic (Fiber-Rich) Foods
Prebiotics are plant fibers that nourish beneficial gut bacteria and promote microbial diversity. Key sources include:
- Legumes and beans
- Nuts and seeds
- Whole grains
- Fruits and vegetables
- Herbs and spices
Include Probiotic Foods
Regular consumption of fermented foods introduces beneficial microorganisms that support microbial balance:
- Yogurt (unsweetened)
- Kimchi
- Sauerkraut
- Other traditionally fermented foods
Limit Immune-Disrupting Foods
- Ultra-processed foods
- Excess added sugars and sweeteners
- Processed and red meats
According to the American College of Lifestyle Medicine, fiber is the most common nutritional deficiency in the United States, with more than 90% of adults failing to meet recommended intake levels. Adequate fiber intake is essential for immune regulation, inflammation control, and gut barrier integrity
A practical clinical takeaway is to focus less on tracking grams of fiber and more on increasing plant diversity in daily meals.
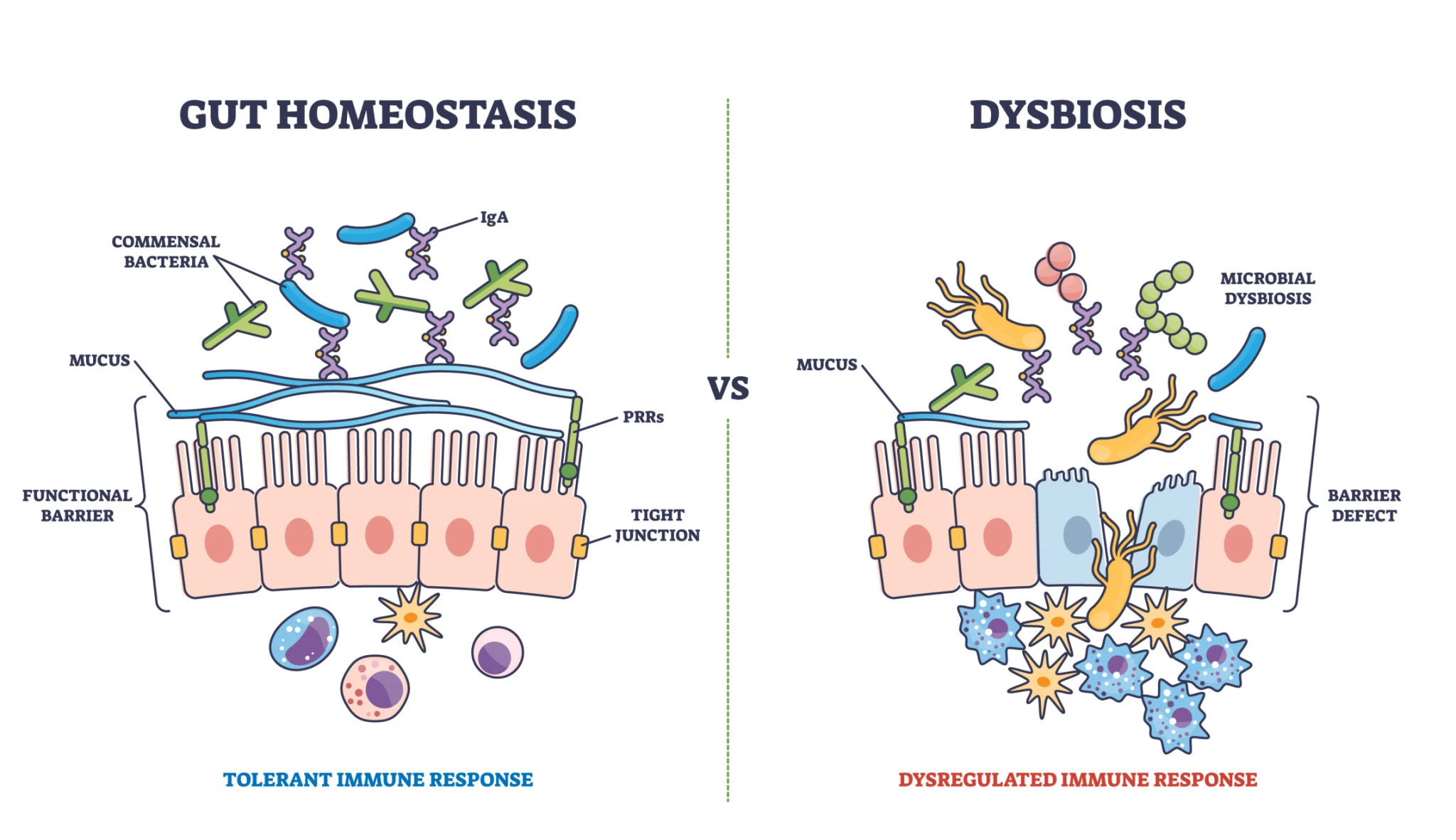
Understanding Intestinal Permeability (“Leaky Gut”)
In Functional Medicine, the term intestinal permeability is used to describe dysfunction of the gut barrier. The intestinal lining acts as a selective filter—allowing nutrients to pass into the bloodstream while preventing toxins, pathogens, and partially digested food particles from entering systemic circulation.
When this barrier becomes compromised:
- Immune activation increases
- Systemic inflammation rises
- Nutrient absorption declines
- Risk of chronic conditions, including autoimmune and inflammatory disorders, increases
Contributors to increased intestinal permeability may include:
- Chronic stress
- Infections
- Antibiotic exposure
- Inflammatory dietary patterns
- Environmental toxins
Importantly, intestinal permeability is not considered a standalone diagnosis. From the Institute for Functional Medicine framework, it is viewed as a downstream effect of underlying root causes, which must be identified and addressed for meaningful healing to occur.
Supporting Gut Restoration
An integrative approach to gut and immune health often includes:
- Targeted dietary changes emphasizing whole, fiber-rich foods
- Strategic use of probiotics and prebiotics when appropriate
- Reduction of immune-disrupting exposures
- Stress regulation and sleep optimization
Functional Medicine clinicians frequently apply the IFM “5 R’s” framework—Remove, Replace, Reinoculate, Repair, and Rebalance—to guide gut restoration and immune recovery.
Lifestyle Medicine Strategies for Immune Resilience
Evidence-based recommendations from the American College of Lifestyle Medicine highlight the following pillars as critical for immune function:
- Nutrition: Diverse, nutrient-dense, whole plant foods
- Physical Activity: Moderate-intensity movement most days of the week
- Sleep: Consistent, restorative sleep (7–9 hours for adults)
- Stress Management: Mindfulness, breathing practices, and relaxation rituals
- Social Connection: Meaningful relationships that reduce stress and support immune signaling
- Avoidance of Risky Substances: Smoking, vaping, and inhaled toxins impair immune defenses
Lifestyle interventions do not guarantee prevention of illness, but they significantly influence immune responsiveness, inflammation levels, and overall health span
Key Takeaways
- Immune health and gut health are inseparable
- The microbiome, gut barrier, and immune system function as an integrated unit
- Daily lifestyle choices shape immune resilience across the lifespan
- Healing the gut supports immune regulation by reducing inflammation rather than suppressing symptoms
By focusing on whole-person, root-cause strategies, we can strengthen immune function and support long-term health and vitality!
Let’s keep adding more life into our years as we add more years into our lives,
~Nhi Do, PA-C, IFMCP, DipACLM
Related Media
- JOY106.3FM Radio Segment – Immune Health Through the Lifespan: https://youtu.be/SUA4JFmrE5M?si=CMR1kGH3aU1OSXqi&t=540
- Visit www.nhimado.org → Media Tab for additional interviews, articles, and resources
- Learn more about research and trusted products for our microbiome: READ this page